Breaking Down Barriers: Depression and Multiple Sclerosis
- Jul 20, 2020
- 6 min read
By Cathleen Julian
Depression is frightfully common in multiple sclerosis, so much so that about half of those with the disease will have at least one major episode. Worse, this depression is not the simple result of being bummed about having MS or coping with increasing disability. Hardly. In fact, fewer than one in five patients with ALS, normally a fatal and devastating disease, suffer from depression, rates far below multiple sclerosis. Why? As psychologist Cathleen Julian (ActiveMSers' newest contributor) explains, MS depression is a different animal. But there is sun behind those clouds.

Years ago I worked as a Rehabilitation Counselor on the Neurology Ward of my county hospital. A man I will call Charles, an in-patient on the neurology ward, had requested guidance about work suited to his current disability level. I was fond of Charles. On the day of what would have been our fifth meeting, I walked into his room and saw that his bed was empty. The staff at the nursing station told me that he had gone home. I had to note the closure of his case and I asked for his chart. The nurses exchanged some uneasy glances and then handed it to me. “Well, you would have heard anyway. Sorry.”
Charles had misled the staff about where he was going, found his way to the laundry room and locked the door from inside. He smashed a plastic detergent bottle apart and used a plastic shard to open an artery in his neck. He lay hidden behind a row of washing machines and bled to death before the staff realized he was not in physical therapy as he had said he would be.
As I read this I broke into tears.
The nurse wanted to comfort me. She touched my arm and said: “Look, honey, he had MS. Sometimes having a set back and being readmitted to the hospital are just way too much to bear.”
"MS depression is a different animal."
“I don’t understand,” I said. “If his story is so familiar, why wasn’t he being protected on the Psych ward?”
“Oh, you are funny. You’ve just finished your Psych rotation and you haven’t yet learned that people who feel worthless often put on a false front? You are not aware that folks get so embarrassed about how they really feel that they fib to their Psychiatrist?”
I was taken aback.
“But there are many patients who have been on this ward for a long time who have even more severe disability than Charles, and they haven’t committed suicide!”
The nurse then educated me on the unique challenges of multiple sclerosis.
“Well, that’s right. It is not as much about disability as about the particular nature of depression in multiple sclerosis. Depression is part of the MS disease process itself. Symptoms of depression in MS are not merely a reaction to MS symptoms. MS involves injuries to the brain where emotions are centered. You may know folks on this ward who are more disabled than Charles. They may have even been disabled a much longer time. But they don’t have MS. People with other chronic illnesses are not as likely to be as deeply depressed as someone with MS. MS depression is a different animal.”
It is a different animal indeed. The statistic “fifty percent of those with MS will experience clinical depression at some point” is often quoted. This statistic almost certainly underrepresents the population of those with both multiple sclerosis and clinical depression. Several factors are involved in this misleading underestimation. Certain symptoms of MS are quite similar to symptoms of clinical depression. It’s not uncommon for both the patient and the clinician to misidentify the source of the symptom. For example, cognitive changes common in MS are also found with clinical depression in those who do not have MS. If the clinician assumes that these cognitive symptoms are due to MS alone, actual clinical depression may go undiagnosed, untreated and undocumented.
The neurology nurse was spot on about another basis for the underestimation of severe depression in MS. Many people with MS do not want to disclose symptoms because they are convinced that they would be revealing a shameful flaw. It is very difficult for someone experiencing the feelings of worthlessness inherent in depression, to realize that those feelings do not reflect reality.
“The risk of suicide is 7.5 times greater for those with MS than for people who do not have MS.” This is another often-quoted statistic about MS-related depression that misrepresents the prevalence of severe depression in MS. Because only “successful” suicides are represented in this statistic, the actual incidence of attempted suicide remains unknown.
Depression is very common in MS. If you are experiencing depression, you are not alone. Far from it. No, you are not the only one who finds no value in life. No, you are not the only one who feels wretched. No, you are not the only one who feels unlovable to the core. No, you are not the only one who feels shame about these feelings.
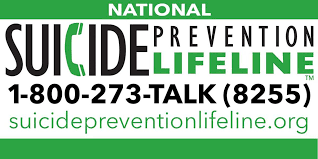
IMPORTANT: The Mayo Clinic breaks down depression, including its symptoms, treatments, therapies, and more. “Medications and psychological counseling (psychotherapy) are very effective for most people with depression.” If you think you may have depression, this is a must-read.
What Depression in Multiple Sclerosis IS:
Extremely common. Depression in MS is very common. You are not alone. Fifty percent is the estimated frequency of at least one episode of major depression during the course of the disease. The actual frequency is very likely much higher than reported.
A threat. The leading cause of death in MS is suicide. Depression exacts a heavy toll on relationships. Couples may break up, due, not to MS itself, but in response to the spiraling, self-reinforcing symptoms of untreated depression
Emotionally painful. For the many who suffer with MS-related depression, shame, despair, and hopelessness remain a near constant. Deeply held convictions of inadequacy and worthlessness derive from the condition of depression.
Disabling. Depression is disabling and magnifies the disabling impact of MS itself. Depression is disabling physically, emotionally and cognitively.
Disabling physically. Depression will amplify the experience of pain, fatigue and physical weakness. Depression often causes physical dis-regulation making coordinated movement more difficult.
Disabling emotionally. Depression can distort feelings and imbue distorted feelings with a sense of absolute truth.
Disabling cognitively. Depression intensifies the cognitive issues of MS. Depression can worsen cognitive slowing, as well as intensify problems with concentration, attention, and memory.
Misunderstood. Despite how common depression in MS actually is, it is frequently misunderstood. General availability of medical knowledge about depression in MS abounds yet it tends to remain a stigmatized condition. It seems to be particularly stigmatized by those who suffer with it. It is difficult indeed to persuade someone who is depressed that depression is not their fault and that they may suffer from being human and fallible but that they are not as ”flawed” as the feel they are .
Treatable. There are many ways of treating depression in MS. Absolutely treatable, as in you will really feel much better.

What Depression in Multiple Sclerosis is NOT
An accurate mirror of your worth. Depression is not a condition that will provide you with reliable and accurate information about your character, your value as a human being, or the worth of your life. Depression is not an infallible mirror reflecting ultimate truths about you. Deeply held convictions about guilt, shame and worthlessness derive from depression. This has to do with the physiological basis of depression. It is possible to create shame and collapse in primates by manipulation of their neurotransmitters and hormones.
An accurate predictor of the future.
A trustworthy guide to the validity of your shame. It is not a failure of courage. It is not a flaw in your character or a failure of will or a failure of anything else! Shame derives from the physiological aspects of brain injury.
A failure of effort. It has as much to do with your effort as a bladder infection. You would not urge somebody who has a bladder infection to “Get out of your own way. You’re in your head too much!” You might say: “Go to a doctor” but not: “You are suffering too much because you have surrendered your will.”
Evidence that only suicide will stop the pain. Treatment will stop the pain. Treatment will not stop the inevitable pain of living real life but it will end the relentless suffering of self-loathing, deepening sadness and despair.
Evidence that you should die for the sake of others. Recognize your deep conviction that death would save others from pain for what it is: The horrible and erroneous conviction of someone who has suffered too deeply for far too long.
ABSOLUTELY NO ONE WILL BE BETTER OFF WITH YOU DEAD.

I enjoy sharing informative healthcare topics that help people better understand medical services. Recently, I’ve been exploring how types of doctors can guide patients in choosing the right specialist for their condition, whether it’s a primary care physician, surgeon, or diagnostic expert. My focus is on clear education that improves awareness and supports confident healthcare decisions
In research-intensive universities, a university lecturer frequently applies for research grants to fund projects and student involvement. Successful grant acquisition supports team building and resource acquisition. Publication of findings contributes to the discipline’s body of knowledge. UNICCM explains that research grant competitiveness is a core academic skill.
This article really highlights how depression in MS is more than just sadness. It's a complex issue. On a different note, I recently used an online angle measurement tool for a DIY project, and it made things so much easier. Thanks for sharing this important info!
IWIN mang đến hành trình giải trí đẳng cấp với nền tảng công nghệ tiên tiến và kho trò chơi hấp dẫn. Thương hiệu IWINCLUB luôn tiên phong trong việc nâng cao trải nghiệm người dùng. Truy cập iwinclub ru com ngay hôm nay để tận hưởng khuyến mãi cực khủng và không gian cá cược hàng đầu!
Khẳng định vị thế hàng đầu, Luck8 xây dựng nền tảng luck8net com tối ưu cho người Việt. Với giao diện trực quan, tốc độ nhanh, bạn có thể dễ dàng theo dõi thông tin tại https://luck8net.com/ để bắt đầu trải nghiệm ngay hôm nay.